By the doctor Isabelle Rousseaux
For 10 years, I have monitored and analysed the side-effects encountered after hyaluronic acid injections. Sometimes the cause is clear, but other times it remains a mystery. The pandemic has greatly changed the patient profiles and we are seeing a lot fewer side effects.

A brief history
The problems began when the syringe and needle were invented in 1844-1853 and people started looking for products to inject in order to correct imperfections and the signs of aging: paraffin, oil, silicone, seaweed, plastic, etc.
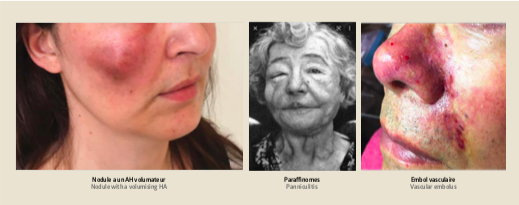
Things looked promising at the beginning, but we should have suspected that the skin would react upon injection of a foreign body (photos). Silicone was banned in 1997, Dermalive in 2007 and Novabel in 2010. Hyaluronic acid (approved for use in 1994) has all of the virtues of the perfect injectable product except that, in order to ensure its longevity post-injection, it needs transforming, and therefore its properties vary.
Two side-effects have emerged with the evolution of injection techniques and the technology of the products: vascular emboli in the arteries and nodules.
HA emboli can appear after the accidental injection of the product into an artery, regardless of the site. The after-effects can be dramatic, such as a loss of vision, but the prognosis is generally good in France as, firstly, we have a better understanding of this adverse effect and, secondly, we are now authorised to use hyaluronidase to dissolve the embolus.
Nodules can sometimes appear very quickly. They can be inflammatory if there is a conflict of myomodulation, or non-inflammatory in the case of excess product. Most often, they are inflammatory nodules that appear later on, a few months after injection.
We try to connect the cause with a change in the patient’s immunity:
- Known hypersensitivity to hyaluronic acid or lidocaine
- Sarcoidosis, scleroderma, annular granuloma, haemorrhagic recto colitis
- Active autoimmune disease
- Serious illness that is being treated
- Pregnancy, breastfeeding, children
- Presence of a non-resorbable implant in the injection site
We also look for:
• Illnesses connected with immune or inflammatory issues
• Infections in or outside the injection site: dental, viral
• High stress levels, severe vexation
• Areas subjected to myomodulation, like the masseters
For years, I have been called upon to treat the side-effects of filler injections and these calls, which I used to receive once or twice a week, have now been reduced to once or twice a month. This is because fewer injections were performed during the lockdowns, but also because more precautions are being taken in terms of hygiene, the questions asked, and the amounts injected. The guidelines are strict with regard to the time left between vaccination and injection, and in terms of counterindications: viruses, infections and inflammation.
A few questions to ask before injecting, in addition to the usual counterindications:
• How many Covid vaccinations have you had and when?
• Are you planning any holidays?
• Do you play any wind instruments or sing in a choir?
• Do you grind your teeth?
• Are you currently having any dental treatment, do you have any dental problems?
And above all:
• Check the counterindications before every injection
• Know when to say no
• Inject small amounts at a time
• Inject gently, slowly
• Cause as little pain as possible
• Disinfect before and after every injection
Hyaluronic acid injections should be carried out by a qualified doctor who is well trained in this technique and who is, above all, capable of dealing with any potential side-effects.
 By the doctor Isabelle Rousseaux
By the doctor Isabelle Rousseaux
Aesthetic dermatologist; board member for the syndicate of dermatologists and training manager for assistants;
board member of the gDEC.
President of Defee Nord.
Consultant doctor for side-effects for Allergan.
More information on lillecotesud.fr